Menopause is a stage in a woman’s life, usually between the ages of 45 and 55, when the physiological cycle of menstruation and ovarian function ends and reproductive capacity permanently ceases. According to the World Health Organization, a woman is considered to be in menopause when 12 months have passed since her last menstruation. Menopause can also occur following surgery (when both ovaries are removed) or medical treatment, in which case it is called induced menopause (surgical or medical).
Stay with us to answer the most important questions about menopause, explaining its differences, symptoms, and underlying physical and biochemical changes. As specialists in the formulation of nutritional supplements, we will introduce you to the natural solutions that phytotherapy offers to help women through this phase, ensuring a transition of maximum well-being. We will also tell you about Menovon, a dietary supplement that is the result of an exhaustive literature review of ingredients available in modern phytotherapy that have generated positive results in the management of climacteric symptoms. This article may seem long, but with the information we are about to give you, we are sure you will have a clearer idea of what happens during menopause and why Menovon might be your next supplement.
Why does menopause occur?
In a nutshell, we can say that menopause is the permanent cessation of menstruation. This process begins because the structures called follicles in the ovaries become depleted. These ovarian follicles are responsible for the production of female hormones, which are responsible for the menstrual cycle.
Ovarian function
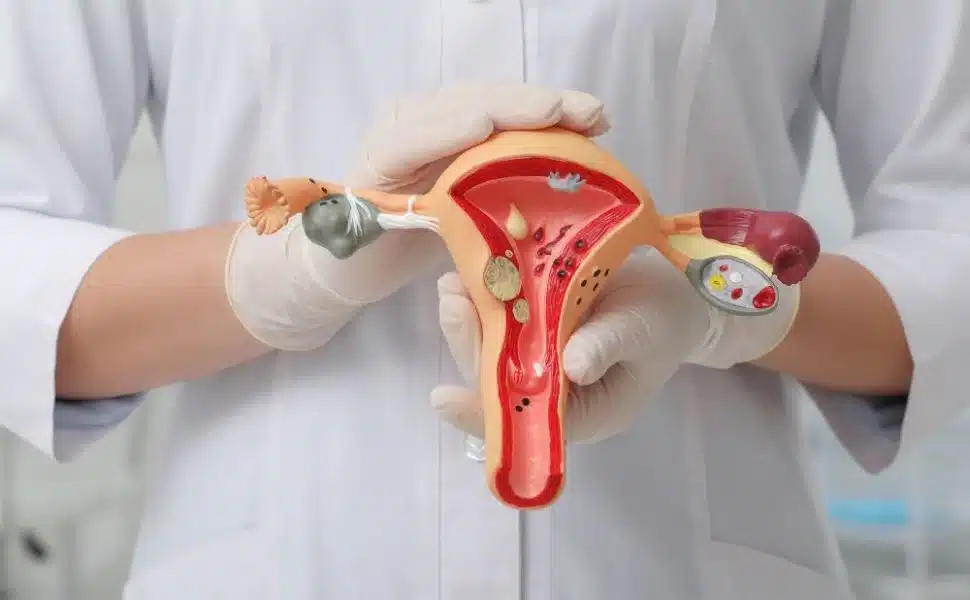
Ovules are the sex cells, carrying the genetic load that a woman passes on to her children. They grow and mature in ovarian follicles. There are numerous follicles in the ovaries, but every 28 days only one follicle develops and results in the formation of a mature ovum. This egg will travel along one of the fallopian tubes to the uterus. If it is fertilized by a sperm on the way, it will form an embryo that can implant in the uterus, resulting in pregnancy. If it is not fertilized, the egg will degenerate and be shed in the next menstrual period.
Ovarian follicles are produced by the woman herself before birth. Only nine weeks after conception, female fetuses begin to produce ovarian follicles. Each follicle is responsible for the development of a single immature egg (oocyte) within it. At birth, women have a limited ovarian endowment of about one million oocytes, which decreases over the course of life. By the time of puberty, this number is reduced to about 400,000 to 500,000. In each of the menstrual cycles that begin month after month from this time onward, only about 400-500 oocytes will reach ovulation and the rest will degenerate along the way.
Ovarian follicles also have another important function, that of producing the female sex hormones estrogen and progesterone from cholesterol. These hormones control menstrual cycles, fertility, and pregnancy. They are also essential for the development of female sexual characteristics. In addition to reproduction and pregnancy, estrogens have other important functions that make them critical to women’s health and well-being. They are involved in fat and cholesterol metabolism 1, the synthesis of neurotransmitters such as adrenaline, norepinephrine, dopamine and serotonin 2, 3, bone tissue metabolism 4, collagen production 5, blood pressure control 6 and, together with androgens, they stimulate libido. 7
As the years go by, there is a gradual decrease in the number of available ovarian follicles. Around the time of menopause, the number of follicles is already greatly reduced and they produce almost no female hormones. This deficit of estrogen and progesterone can cause serious health problems, especially in the case of estrogen, because of the important functions this hormone performs beyond the menstrual and reproductive cycle.
What is the difference between menopause and climacteric?
Strictly speaking, menopause refers to a woman’s last menstrual cycle, just as menarche refers to the first. However, it is very common to use the term menopause to refer to the years before and after this particular physiological event, although it is more correct to use the term climacteric, a word derived from the Greek κλιμακτήρ(klimakter), meaning steps or rungs. We can divide climacteric into 3 typical stages:
The stages of menopause
Perimenopause: a period of time when the hormone production of the ovaries is already greatly reduced and continues to decline gradually. This is due to a decrease in the number of available ovarian follicles. During this period, the ovaries become smaller and lighter, while the blood vessels supplying them atrophy. There are fewer and fewer follicles remaining and sometimes they do not mature each cycle, so menstrual cycles without ovulation (anovulatory) occur. During late perimenopause, menstrual cycles become increasingly irregular, with a general tendency toward longer cycles (menstruation does not occur every month). It is during perimenopause that the first symptoms of climacteric occur.
Menopause: a woman’s last menstrual cycle. Because menstruation becomes less frequent during late perimenopause, menopause is diagnosed retrospectively by counting the 12 consecutive months of no menstruation (amenorrhea) since the last menstruation.
Postmenopause: begins with the end of perimenopause and is usually considered over around age 65. Follicles have stopped functioning, ovarian function has ceased, and hormone production is virtually absent. Estradiol and progesterone concentrations are very low. The ovarian stroma continues to produce testosterone, so the ratio of estrogen to androgen changes. In some cases, this may result in the appearance of signs of hirsutism (excessive hair growth in women). Complications and symptoms due to estrogen deficiency appear at this stage, which will manifest slowly and gradually over the years.
What are the typical symptoms of climacteric?

During climacteric, women undergo a series of physiological and psychological changes that, in some cases, may give rise to symptoms such as: 8
- less frequent menstruation that eventually stops.
- strong or accelerated heartbeat (palpitations)
- hot flashes, which usually worsen in the first 1-2 years after menopause.
- night sweats
- redness of the skin
- sleep problems (insomnia)
- more frequent headaches
- mood changes, including irritability, depression and anxiety
- forgetfulness (in some women)
- vaginal dryness and painful intercourse (dyspareunia)
- decreased sexual interest or changes in sexual response
- recurrent urinary tract infections
- urinary incontinence
- joint pain
- osteoporosis
It is important to note that not all women experience the same symptoms and with the same intensity. Moreover, they may develop at different stages of the climacteric period.
What is behind climacteric symptoms?
Estrogen deficiency is reflected in the urogenital (urinary and genital) system. Because estrogen participates in collagen formation in skin, mucous membranes, and connective tissue, its deficiency results in a significant decrease in elasticity and tensile strength. 5 Therefore, the decrease in collagen during climacteric will be largely responsible for the symptoms of joint pain, urinary incontinence, recurrent urinary tract infections, and dyspareunia (painful intercourse).
Osteoporosis is an important risk factor in postmenopause. Estrogen promotes calcium absorption in the gut by stimulating specific receptors in the osteoblast, activating bone matrix production and calcium deposition in bone. 9 The greatest loss of bone mass occurs in the five years following menopause. 10
Estrogen is known to contribute to increased levels of HDL cholesterol (good cholesterol) and reduced levels of LDL cholesterol (bad cholesterol). In addition, they are involved in all stages of atheroma plaque inhibition with their anti-inflammatory role. 11 All this results in lower cardiovascular risk for premenopausal women, compared with men of the same age. However, postmenopausal women lose this protective estrogen factor and thus tend to have higher levels of total cholesterol, LDL cholesterol, triglycerides, and lower levels of HDL cholesterol. 12
Due to their role in the synthesis of certain neurotransmitters, estrogen is beneficial for cognitive and psychoaffective functions, mood, and memory. Therefore, menopause is often associated with mood changes, including increased irritability, increased susceptibility to depression and anxiety attacks. 13
How do doctors diagnose menopause?
The climacteric symptoms, already mentioned, are usually enough to let most women know that the transition to menopause has begun. If you have concerns about irregular menstruation or hot flashes, consult your doctor. In some cases, your doctor may recommend additional tests. In some cases, your doctor may recommend blood tests to check levels of markers such asluteinizing hormone (LH),follicle stimulating hormone (FSH), andestradiol.
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH), produced by the pituitary gland (located at the base of the brain), are the hormones responsible for stimulating the production of estrogen and progesterone by ovarian follicles. When estrogen and progesterone levels are reduced due to a lack of follicles, the hypothalamus (a region of the brain that acts like a gland) releases more gonadotropin-releasing hormone (GnRh) to signal the pituitary gland to produce more FSH and LH, in an attempt to “force” the ovary to produce more estrogen or progesterone. But the problem is that there are no longer enough ovarian follicles to produce them. As a result, FSH and LH remain elevated and are then used as analytical markers to confirm entry into menopause.
Estradiol is the main form of estrogen present in premenopausal women. After menopause, its levels decrease significantly, making estradiol another important analytical marker of menopause.
What treatments are available for menopausal symptoms?
Treatment of climacteric symptoms aims to provide estrogen exogenously to compensate for deficient endogenous production. This is called hormone restoration therapy or hormone replacement therapy. The problem with this therapy is that it increases the risk of endometrial cancer. 14 This risk can be reduced by adding a progestin to the treatment, although this increases the risk of breast cancer. 14, 15 For all these reasons, there are concerns about the use of chronic hormone restorative therapy in women with mild symptoms. In this case, preventive treatment with herbal medicines is an increasingly popular alternative.
Many epidemiological studies have verified the efficacy of phytotherapeutic preparations for the management of menopausal symptoms and the prevention of any cardiovascular or osteoporosis problems in healthy, asymptomatic women. 14 Further evidence for the effectiveness of phytotherapy is the fact that populations with diets rich in isoflavones have a lower incidence of climacteric symptomatology, particularly hot flashes. Hot flashes are the most common symptom of menopause and are experienced by about 75-85% of Western women, while only 15-25% of Japanese women experience hot flashes. 14
Consumption of soy, a food rich in isoflavones, is a feature of the diet of Far Eastern countries, such as eastern China and Japan.
Supplements for menopause?
The answer is yes. Through dietary supplements we can gain the benefits of nutrition (vitamins, minerals and macronutrients) and herbal medicine (medicinal plants) for the management of climacteric symptoms.
Some plants have substances with molecular structures similar to steroid hormones, giving them mild estrogenic and antiestrogenic properties. Other plants do not have estrogenic action, but have active components that act at the level of neurotransmitters, helping to reduce typical climacteric symptoms. According to several epidemiological studies, these plants help to avoid the discomforts of menopause, without the side effects that can occur as a result of hormone therapy. 14
A healthy, balanced diet is essential and, in principle, will provide you with all the nutrients you need during this transitional period. However, it should be noted that certain vitamins are particularly important during this phase, and if you cannot ensure a daily supply of these nutrients through your diet, dietary supplements can help.
Menovon: a dietary supplement for menopause
Motivated by the need to help women during this important period, our team of specialists developed Menovon. Its formula is the result of a comprehensive literature review of advances in herbal medicine and nutrition to help manage climacteric symptoms. 16 Menovon combines the action of soy isoflavones and red clover extracts, with black cohosh and chasteberry extracts and vitamins E, D3 and B6. Its formula is 100 percent natural, with no synthetic additives or artificial preservatives.
Stay with us to learn how Menovon’s ingredients can help you experience a peaceful and comfortable menopause. We will also introduce you to 3 other dietary supplements that we recommend along with Menovon that can help you have a peaceful and comfortable menopause.
Phytoestrogens from soy and red clover

(Soybean)
Phytoestrogens are naturally occurring nonsteroidal compounds found in many foods. The three main classes of phytoestrogens are isoflavones, lignans, and coumestans. Of these, isoflavones, found mainly in soybean(Glycine max), red clover(Trifolium pratense) and other legumes, are the most important because of their mild estrogenic activity. 17
Due to their structural similarity to the body’s estrogen, phytoestrogens are able to bind to the same cellular receptors used by estrogen in the body, thus showing some estrogenic activity, which can help combat the discomforts of menopause without the side effects that can occur as a consequence of hormone therapy. 14, 18 In fact, the estrogenic activity of isoflavones is the most studied as a natural alternative to hormone treatments. 19
Isoflavones occur naturally in their inactive glycosylated form, that is, as precursors. Only after ingestion, through the enzymatic action of intestinal bacteria, do they lose the glucose molecule and transform into the active forms. 20

(Red clover)
There are two types of cellular receptors for estrogen in the human body . Receptors alpha (ER-α) are distributed in the central nervous system, endometrium, breast and liver. Receptors beta (ER-β) are located mainly in bone, the vascular wall, the urogenital tract and also in the central nervous system. However, isoflavones have been shown to have a higher affinity for the beta-β receptor, so their action is more pronounced in those target organs and tissues where beta-β receptors predominate, such as the central nervous system, skeleton, vascular wall, and urogenital tract. Because they have virtually no action on ER-α receptors, isoflavones have no significant effects on breast and endometrial tissue proliferation. 19
ER-α and ER-β receptors are proteins located within cells that act as specific receptors for estrogen. These receptors stimulate cell multiplication and are “critical” mediators of a variety of organ-specific biological processes in the human body.
Isoflavones also have antioxidant action, which results in protection of the vascular wall by reducing oxidation of LDL cholesterol. They also act as antiplatelet agents by inhibiting the binding of thromboxane A2 to its platelet receptor. 14
Soybean and red clover share the same isoflavones but in different proportions, which may explain some differences in the results of clinical trials. 21 In order not to make this article too long and technical, we will not dwell on the structural differences between soybean and red clover isoflavones. If you are interested in this issue, we recommend a review article published in 2006 in the scientific journal Climateric, by researchers from the Department of Obstetrics and Gynecology at the University of Illinois College of Medicine in the United States. In this article, the researchers discuss the different isoflavone profile of soybean and red clover and how this may explain the different clinical trial results. For example, regarding the observed effects on lipid profile, soy extract produced better results in reducing total cholesterol and LDL cholesterol levels, while red clover extract produced greater reductions in triglyceride levels and increased HDL cholesterol levels. 21
An optimal dose of isoflavones has not been standardized in clinical trials for the management of climacteric symptoms. However, in most of these studies, the optimal amounts of total isoflavones to observe a positive effect were about 40-50 mg per day. 22
Each daily dose of Menovon provides 40 mg of isoflavones, from extracts of soybean (50 mg extract standardized to 40 percent isoflavones) and red clover (250 mg extract standardized to 8 percent isoflavones).
Black cohosh

Black cohosh(Cimicifuga racemosa) is a perennial herb native to the United States and Canada, traditionally used to relieve dysmenorrhea, during labor, and to relieve climacteric symptoms. 23 Several studies have demonstrated the efficacy of black cohosh extracts for the relief of various symptoms associated with menopause, such as vasomotor symptoms (hot flashes, night sweats) and psychic symptoms (mood swings, irritability, sleep disturbances). 16, 23
In the past, the efficacy of black cohosh preparations in relieving menopausal symptoms was thought to be related to the presence of phytoestrogens, such as isoflavones from soybean and red clover. However, several in vitro and in vivo studies have shown that this is not true. The components of black cohosh extracts do not bind to estrogen receptors and therefore do not exert a direct estrogenic effect. 24 More recent studies indicate that some of the components of black cohosh extract, probably triterpene glycosides, activate specific serotonin receptors located in the hypothalamus, exerting a serotonin-like action. 25, 26
This is important because during menopause there is a drastic decrease in serotonin levels in the body due to the lack of estrogen. 26 With decreased serotonin availability, the body is in a stressful situation. 26 With decreased serotonin availability, many of these receptors are not activated and the hypothalamus is unable to perform its thermoregulatory function properly. The hypothalamus is the neurological center of the body’s thermoregulation. Insufficient activation of these serotonin receptors leads to a shortening of thethermoneutral interval, which is why postmenopausal women are more sensitive to small changes in environmental temperature. 27 The thermoneutral interval is the range of environmental temperatures in which metabolic heat production (by the body) is not affected by environmental temperature. In this interval, body temperature remains constant.
Estrogen promotes the production of an important enzyme in serotonin synthesis, tryptophan hydroxylase, and inhibits the reuptake of serotonin into the synaptic space, promoting its action. 28
Unlike isoflavones, randomized clinical trials with black cohosh extracts are less abundant. 29 However, the available data suggest that black cohosh extracts may be useful for the treatment of vasomotor and psychological symptoms of menopause, as they produced a decrease in the frequency and intensity of these symptoms, as well as an improvement in the quality of life of these patients, without significant adverse effects. 29 The doses used in the studies ranged from 5 to 40 mg per day of black cohosh dry extract.
The Menovon formulation contains 40 mg of black cohosh dry extract, standardized to 2.5 percent triterpene glycosides.
Chasteberry or chasteberry

Chasteberry (Vitex agnus-castus L.), also known as vitex, chasteberry or friar’s pepper, is a plant native to the Mediterranean basin and East Asia. The fruit of this plant has been used since ancient times for a wide variety of gynecological disorders. In the Middle Ages it was considered the plant of chastity, as it was believed to decrease libido and help monks suppress sexual desire. More recently, in Europe, chasteberry has again been in demand for the management of PMS symptoms. Indeed, the pharmacological activity of chasteberry has been demonstrated by numerous clinical studies, particularly in the treatment of symptoms related to corpus luteum insufficiency, such as menstrual cycle irregularities, menstrual dysfunction, mastopathy (breast pain), and premenstrual syndrome.
The extract of the chasteberry fruit contains a broad spectrum of active compounds such as flavonoids (including vitexin and casticin), terpenoids, and essential oils. 30 The combination of active compounds present in the fruit extract has demonstrated greater therapeutic activity than each of these compounds in isolation. 30 Studies suggest that some of these compounds, probably the terpenoids, act by decreasing prolactin hormone levels through their interaction with D2-type dopaminergic cell receptors in the pituitary gland. 31, 32 In other words, these active compounds mimic the action of dopamine. Excessive prolactin production (hyperprolactinemia) causes a deficit in progesterone production, resulting in an imbalance between estrogen and progesterone, leading to symptoms related to corpus luteum insufficiency. 32
Some components of chasteberry have also been shown to increase melatonin secretion, 33 and can bind to beta-opioid and estrogen (beta-β-β) receptors. This explains the increased production of endogenous endorphins and their weak phytoestrogenic activity.
The use of agnocaste for the treatment of climacteric symptoms is more recent and, as a result, there are not many published clinical studies available with a specific focus on menopause. However, as with premenstrual syndrome, hormone balance, increased melatonin production, and estrogenic action are important properties for the management of climacteric symptoms. 34 Indeed, early clinical studies in women in the climacteric period indicate that agnocaste improves symptoms such as hot flashes, mood, and sleep quality. 35
In particular, the German E Commission approves its use for menstrual cycle irregularities and premenstrual syndrome (PMS) and it is widely prescribed by German family physicians and gynecologists.
Menovon also contains 30 mg of chasteberry extract, also known as agnocaste, standardized to 0.5 percent vitexin.
Vitamin E
Vitamin E groups several isomers, including tocopherols and tocotrienols. The term isomer indicates that these are compounds with the same molecular formula (in terms of number and type of atoms), but with a different structural formula and therefore different properties. Alpha-tocopherol is the most common isomer in nature and the one with the strongest vitamin action. As a lipid (fat-soluble) vitamin, vitamin E is able to bind to the lipid part of cell membranes, protecting their phospholipids from oxidative stress. Vitamin E sequesters free radicals, reducing them to less active metabolites. Vitamin E is therefore essential for the proper functioning of all cells in the body.
Oxidative stress is also involved in the pathogenesis of menopausal symptoms, such as vasomotor disturbances (hot flashes and night sweats). During the menopausal transition and in the postmenopausal period, women experience repeated episodes of vasomotor disturbances, resulting in increased metabolic rate. 36, 37 These episodes contribute to oxidative stress through increased levels of oxidative species in the body. At the same time, with aging, the level of antioxidant substances in the body decreases, making a woman’s body more susceptible to various age-related diseases. 36 This decrease in antioxidant levels, combined with the gradual loss of estrogen in the female reproductive system, is closely related to the various sequelae of menopause, such as heart disease, vasomotor disorders, and osteoporosis. 36
Menovon formula also contains 12 mg of vitamin E, in the form of alpha-tocopherol, ensuring a daily intake equivalent to 100 percent of the recommended daily allowance for this vitamin.
Vitamin D

Bone is a very active structure. A continuous process, called bone remodeling, involves constant resorption (osteoclastic activity) and formation (osteoblastic activity) of bone. Estrogen increases the amount of vitamin D receptors on osteoblasts. 38 These receptors control osteoblast function, promoting bone formation. Vitamin D deficiency, combined with decreased estrogen production during the climacteric period, produces a marked decrease in osteoblastic activity, which is reflected in reduced bone mineral density (osteoporosis) and an elevated risk of fractures. 39
Vitamin D regulates an important enzyme in the transformation of tryptophan to serotonin, tryptophan hydroxylase 2 (TPH2). As mentioned above, serotonin is a neurotransmitter involved in the body’s control of emotions, mood, and thermoregulation. Therefore, its decrease during the climacteric period may be related to vasomotor symptoms (hot flashes and night sweats) and mood swings. 25, 26 It should be noted that melatonin, the sleep hormone, is produced from serotonin, and therefore vitamin D deficiency may affect sleep quality. In fact, vitamin D supplementation has been associated with improved mood in women during the menopausal transition period. 40-43
Vitamin D is also a fat-soluble vitamin and is stored mainly in the liver and adipose tissue. It is represented by two fat-soluble compounds: vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). Cholecalciferol is the most active form of vitamin D due to its more efficient conversion to calcifediol in the liver. In fact, most studies show that vitamin D3 is more effective than vitamin D2 in increasing calcifediol levels in the blood. 44, 45 The potency of vitamin D2 is less than one-third that of vitamin D3. 45
Vitamin D is another active ingredient in the Menovon formula. Each dose provides 200 IU of vitamin D3 (cholecalciferol), which is 100 percent of the recommended daily allowance for this vitamin.
Vitamin B6
In addition to vitamin D, serotonin synthesis requires vitamin B6. This vitamin is an important cofactor of another enzyme involved in serotonin synthesis, L-aromatic amino acid decarboxylase (AADC). For this reason, adequate intake of vitamin B6 and D is important for the control of vasomotor symptoms of the climacteric period, for a better feeling of well-being, and for sleep quality.
Vitamin B6 has other important functions in the body, such as controlling protein metabolism, hemoglobin formation, antibody production, and DNA synthesis. Vitamin B6 is essential for the synthesis of other neurotransmitters such as dopamine, norepinephrine, histamine, glycine, and d-serine, which, together with serotonin, are essential for cognitive function. 46
Unlike vitamins D and E, vitamin B6 is a water-soluble vitamin. Water-soluble vitamins dissolve in water and cannot be stored by the body. Residual amounts of vitamin B6 are eliminated from the body through urine. Although the body maintains a small reserve of water-soluble vitamins, regular intake is necessary.
Menovon contains 1.4 mg of vitamin B6, which is 100 percent of the recommended daily allowance. Menovon can help manage menopausal symptoms. Its carefully selected combination of plant extracts and vitamins is designed to help you overcome climacteric symptoms so that you can experience a peaceful and comfortable menopause. We also recommend 3 other Nutribiolite products that will provide you with additional protection and other important nutrients for this stage of your life. Below we explain what these products are and why we recommend them.
Extra protection and support for menopause
MAG-FUSION is the perfect fusion of essential nutrients during the climacteric period. MAG-FUSION combines magnesium citrate with a selection of 4 vitamins-D3, B6, B9, and B12-that work synergistically to maintain healthy brain function, combat stress, fatigue, chronic muscle pain, and help maintain strong bones and normal homocysteine levels.
In addition to the special selection of vitamins and magnesium, a feature of MAG-FUSION is the use of all these nutrients in their most bioactive forms. For example, MAG-FUSION contains (6S)-5-methyltetrahydrofolate (5-MTHF). This is the bioactive form of vitamin B9. The other forms must be digested in the intestine by the enzyme dihydrofolate reductase (DHFR) to be converted to 5-MTHF. In addition, 5-MTHF is present in MAG-FUSION in the form of the glucosamine salt 5-MTHF, also known as fourth-generation folate or Quatrefolic®. Laboratory studies have shown that this patented form is 1.8 times more absorbable than calcium (6S)-5-methyltetrahydrofolate, the chemical form of 5-MTHF used in other dietary supplements. 53
The combination of omega-3 with vitamins D3 and K2 is essential for various metabolic processes and is critical for the immune, muscular, neuronal, skeletal, and circulatory systems. It also acts on inflammation-reducing processes with a crucial impact on joint protection.
Omega-3 fatty acids have been shown to play an important therapeutic role in alleviating joint inflammation and promoting tissue regeneration of bone and cartilage. Vitamin K2 and Omega-3 help the proper functioning of the cardiovascular system, and vitamin K2 contributes to normal blood clotting. Vitamins D3 and K2 together ensure that calcium is easily absorbed and reaches the bone mass, preventing calcification of the arteries and helping to maintain healthy bones and teeth. These two vitamins also ensure proper functioning of the immune system and support muscle function.
The OMEGA 3+ D3 +K2 ingredients in Nutribiolite are of the highest quality. The omega-3s come from renewably sourced fish oil and are 80% concentrated in total omega-3s, including 50% in EPA (eicosapentaenoic acid) (500 mg) and 25% in DHA (docosahexaenoic acid) (250 mg). Vitamin D is in the form of vitamin D3 and vitamin K2 in the encapsulated form of menaquinone-7 (MK-7 or K2-7), the most bioactive form of this vitamin.
The resulting estrogen deficiency of menopause causes a decrease in skin collagen 5, resulting in a significant reduction in vaginal tissue flexibility, decreased mucosal lubrication, and increased vaginal pH. 47 This combination makes postmenopausal women much more prone to develop repeated urinary tract infections.
Uritractin is a dietary supplement that combines extracts of American cranberry(Vaccinium macrocarpon) and hibiscus(Hibiscus sabdariffa) flowers to help prevent urinary tract infections. (Studies) the antibacterial and antifungal properties of
Proanthocyanidins in cranberry extract are known to prevent bacteria, such asE. coli, from adhering to the inner walls of the urinary tract. Escherichia coli urinary tract infection is the most common infection caused by Escherichia coli. 48
According to several studies, the natural polyphenols in hibiscus extract prevent the formation of fungal biofilms, which are essential for blocking the colonization and reproduction of these pathogens in the urinary tract. 49-51 Hibiscus extract also has antioxidant and diuretic properties that contribute to the proper functioning of the urinary tract.
Serotonin levels decrease during menopause, which is associated with mood changes, sleep disturbances, and decreased libido. 52 Several studies indicate that estrogen regulates the production of the enzyme tryptophan hydroxylase (TPH) 28, an important enzyme in serotonin biosynthesis. TPH catalyzes the limiting step in serotonin production, which is the conversion of tryptophan to 5-HTP. Low estrogen levels may decrease TPH enzyme production and affect serotonin levels.
4Sleep is a dietary supplement that combines 5-HTP (obtained from Griffonia simplicifolia seeds) with melatonin and extracts of valerian root and chamomile flowers in an effective formula to promote biological processes associated with relaxation, improving sleep quality and reducing the time it takes to fall asleep. 4Sleep directly delivers 5-HTP, an excellent serotonin precursor supplement, as it does not require the action of the TPH enzyme.
References
- Cauley, J.A., et al, Menopausal estrogen use, high density lipoprotein cholesterol subfractions and liver function. Atherosclerosis, 1983. 49(1): p. 31-9.
- Del Rio, J.P., et al, Steroid hormones and their action in the female brain: the importance of hormonal balance. Frontiers in Public Health, 2018. 6.
- Torres Jiménez, A.P. and J.M. Torres Rincón, Climaterio y menopausia. Revista de la Facultad de Medicina (Mexico), 2018. 61: p. 51-58.
- Khosla, S., M.J. Oursler, and D.G. Monroe, Estrogens and the skeleton. Trends Endocrinol Metab, 2012. 23(11): p. 576-81.
- Brincat, M.P., Y.M. Baron, and R. Galea, Estrogens and the skin. Climacteric, 2005. 8(2): p. 110-23.
- Maas, A.H. and H.R. Franke, The health of menopausal women with a focus on hypertension. Neth Heart J, 2009. 17(2): p. 68-72.
- Beard, M.K. and L.R. Curtis, Libido, menopause and estrogen replacement therapy. Postgrad Med, 1989. 86(1): p. 225-8.
- National Library of Medicine. Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. A.D.A.M. editorial team. Revision date 13/7/2021.
- Aguilera, J.R., P.G. Ríos, and A.S. Zepeda, Calcium and vitamin D in the climacteric patient. Perinatology and Human Reproduction, 2004. 51(2): p. 83-87.
- PÉRez MartÍN, A., et al, Effect of age and menopause on bone mass. REEMO, 2006. 15(4): p. 57-62.
- Burke, A.P., et al, Effect of menopause on plaque morphological characteristics in coronary atherosclerosis. Am Heart J, 2001. 141(2 Suppl): p. S58-62.
- Reslan, O.M. and R.A. Khalil, Vascular effects of estrogenic menopausal hormone therapy. Rev Recent Clin Trials, 2012. 7(1): p. 47-70.
- Shors, T.J. and B. Leuner, Estrogen-mediated effects on depression and memory formation in women. J Affect Disord, 2003. 74(1): p. 85-96.
- Pérez Alcázar, M., Menopause. Transición. Farmacia Profesional, 2002. 16(9): p. 88-95.
- Candanedo-González, F. and E. Pérez-Salazar, El papel de la progesterona en cáncer de mama. Gaceta Mexicana de Oncología, 2012. 11(3): p. 182-188.
- Excerpted from EFSA’s list of health claim applications under evaluation: ID 4006 – Cimicifuga racemosa (Actea racemosa) (Common name: Black Cohosh) – Menopause: helps maintain a peaceful and comfortable menopause/helps women cope with teltal signs associated with menopause, such as hot flashes, sweating, restlessness, and irritability.
- Cheng, G., et al, Treatment with isoflavones for acute menopausal symptoms. Menopause, 2007. 14(3 Pt 1): p. 468-73.
- Excerpted from EFSA’s list of health claims, under review: ID 4146 – Trifolium pratense (common name: red clover) – Helps maintain a peaceful and comfortable menopause/helps women cope with teltal signs associated with menopause, such as hot flashes, sweating, restlessness and irritability.
- López Luengo, M.T., Fitoestrógenos. Efficacy and safety. Offarm, 2010. 29(3): p. 86-90.
- Gómez-Zorita, S., et al, Scientific evidence supporting the beneficial effects of isoflavones on human health. Nutrients, 2020. 12(12).
- Geller, S.E., and L. Studee, Soy and red clover for middle age and aging. Climacteric, 2006. 9(4): p. 245-263.
- Messina, M., Soy isoflavones deserve greater consideration as a treatment for relieving menopausal hot flashes. Womens Health (Lond), 2014. 10(6): p. 549-53.
- Guo, Y., et al, Traditional uses, phytochemistry, pharmacology and toxicology of the genus Cimicifuga: A review. J Ethnopharmacol, 2017. 209: p. 264-282.
- Wuttke, W. and D. Seidlová-Wuttke, Black cohosh (Cimicifuga racemosa) is a nonestrogenic alternative to hormone replacement therapy. Clinical Phytoscience, 2015. 1(1): p. 12.
- Pachman, D.R., J.M. Jones and C.L. Loprinzi, Management of menopause-associated vasomotor symptoms: Current treatment options, challenges and future directions. Int J Womens Health, 2010. 2: p. 123-35.
- Berendsen, H.H., The role of serotonin in hot flashes. Maturitas, 2000. 36(3): p. 155-64.
- Freedman, R.R., Menopausal hot flashes: mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol, 2014. 142: p. 115-20.
- Rybaczyk, L.A., et al, An overlooked connection: serotonergic mediation of estrogen-related physiology and pathology. BMC Womens Health, 2005. 5: p. 12.
- García-Bienes, H.M. and C.C. Sánchez-Mateo, Cimicifuga racemosa (L.) Nutt. in the treatment of vasomotor symptoms of menopause: a review. Ars Pharmaceutica, 2022. 63: p. 178-188.
- Souto, E.B., et al, Vitex agnus-castus L.: main characteristics and nutraceutical perspectives. Forests, 2020. 11(7): p. 761.
- Heskes, A.M., et al, Biosynthesis of bioactive diterpenoids in the medicinal plant Vitex agnus-castus. Plant J, 2018. 93(5): p. 943-958.
- Haerifar, N., et al, The effect of vitex agnus castus extract on blood prolactin level, sex hormone levels, and histological effects on endometrial tissue in hyperprolactinemic women. Crescent Journal of Medical and Biological Sciences, 2020. 7(4): p. 545-550.
- Dericks-Tan, J. S., P. Schwinn, and C. Hildt, Dose-dependent stimulation of melatonin secretion after Agnus castus administration. Exp Clin Endocrinol Diabetes, 2003. 111(1): p. 44-6.
- Excerpt from EFSA’s list of health claim applications, under evaluation: ID 3654 – Helps maintain physiological well-being during the menstrual cycle. Contributes to female hormone balance during climacteric. Helps relieve menopausal symptoms.
- Chopin Lucks, B., Vitex agnus castus essential oil and menopausal balance: a research update [Complementary Therapies in Nursing and Midwifery 8 (2003) 148-154]. Complement Ther Nurs Midwifery, 2003. 9(3): p. 157-60.
- Doshi, S.B. and A. Agarwal, The role of oxidative stress in menopause. J Midlife Health, 2013. 4(3): p. 140-6.
- Sánchez-Rodríguez, M.A., et al, Association between hot flashes severity and oxidative stress among Mexican postmenopausal women: A cross-sectional study. PLOS ONE, 2019. 14(9): p. e0214264.
- Liel, Y., et al, Evidence that estrogen modulates the activity and increases the number of 1,25-dihydroxyvitamin D receptors in osteoblast-like cells (ROS 17/2.8). Endocrinology, 1992. 130(5): p. 2597-601.
- Ettinger, B., Prevention of osteoporosis: treatment of estradiol deficiency. Obstet Gynecol, 1988. 72(5 Suppl): p. 12s-17s.
- Khan, Q.J., et al, Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat, 2010. 119(1): p. 111-8.
- Jorde, R., et al, Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial. J Intern Med, 2008. 264(6): p. 599-609.
- Lansdowne, A.T. and S.C. Provost, Vitamin D3 improves mood in healthy subjects during winter. Psychopharmacology (Berl), 1998. 135(4): p. 319-23.
- Gloth, F. M., 3rd, W. Alam, and B. Hollis, Vitamin D vs. broad-spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging, 1999. 3(1): p. 5-7.
- Tripkovic, L., et al, Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. Am J Clin Nutr, 2012. 95(6): p. 1357-64.
- Armas, L.A., B.W. Hollis and R.P. Heaney, Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab, 2004. 89(11): p. 5387-91.
- Spinneker, A., et al, Vitamin B6 status, deficiency, and consequences: an overview. Hospital Nutrition, 2007. 22: p. 7-24.
- Tucker, K.M., et al, Vaginal pH: a simple assessment highly correlated with vaginal morphology and symptoms in postmenopausal women. Menopause, 2018. 25(7).
- Pérez-López, F.R., J. Haya, and P. Chedraui, Vaccinium macrocarpon: an attractive option for women with recurrent urinary tract infections and other health benefits. J Obstet Gynaecol Res, 2009. 35(4): p. 630-9.
- Fullerton, M., et al, Determination of the antimicrobial activity of sorrel (Hibiscus sabdariffa) on Escherichia coli O157:H7 isolated from food, veterinary and clinical samples. J Med Food, 2011. 14(9): p. 950-6.
- Dwivedi, M., S. Muralidhar, and D. Saluja, Hibiscus sabdariffa Extract Inhibits Adhesion, Biofilm Initiation and Formation in Candida albicans. Indian J Microbiol, 2020. 60(1): p. 96-106.
- Alshami, I. and A.E. Alharbi,Hibiscus sabdariffa extract inhibits in vitro biofilm formation ability of Candida albicans isolates from recurrent urinary tract infections. Asian Pacific Journal of Tropical Biomedicine, 2014. 4(2): p. 104-108.
- Iturbe, L.A. and B.V.D.d.R. Boada, Menopause and maturity. XVII Online course on pharmaceutical care.
- Miraglia, N., et al, Enhanced oral bioavailability of a new folate salt: comparison with folic acid and a calcium folate salt in a pharmacokinetic study in rats. Minerva Gynecol, 2016. 68(2): p. 99-105.